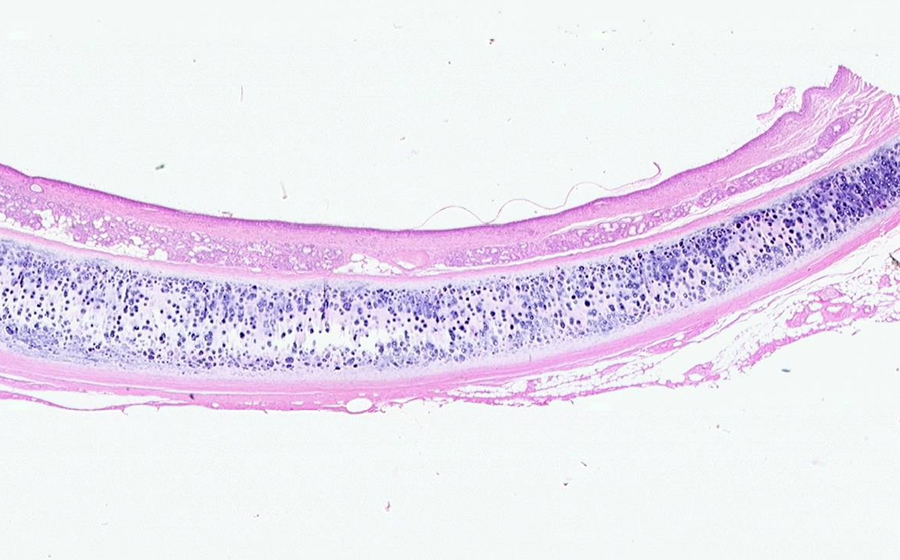
Image 1: Sectioning of the lung reveals cut surfaces that are more solid appearing, rather than spongy. Vague nodules are prominent, and are coalescing/consolidating into larger pale regions. Many of the nodules have bronchioles at their periphery.
Question: In very general terms, what is the expected size and weight of this lung (vs. normal)?
Question: What processes may produce these types of gross features?

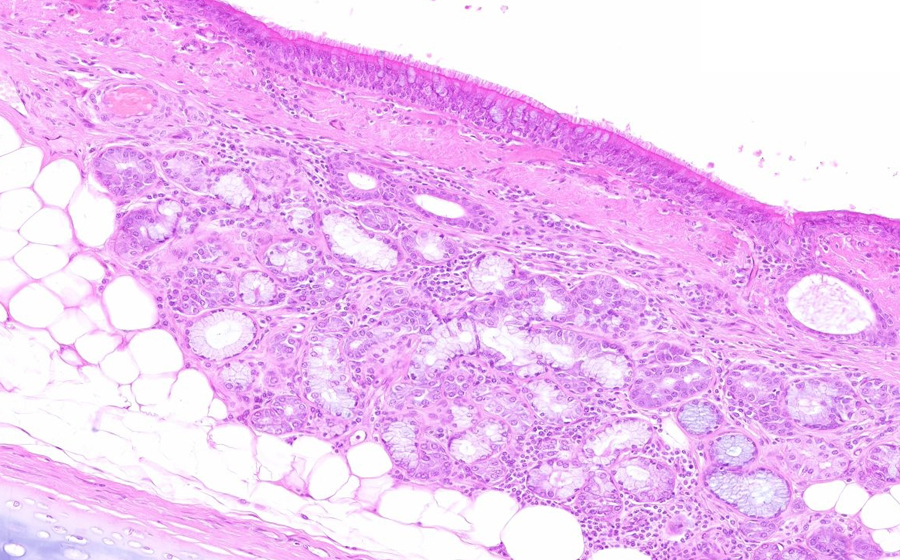
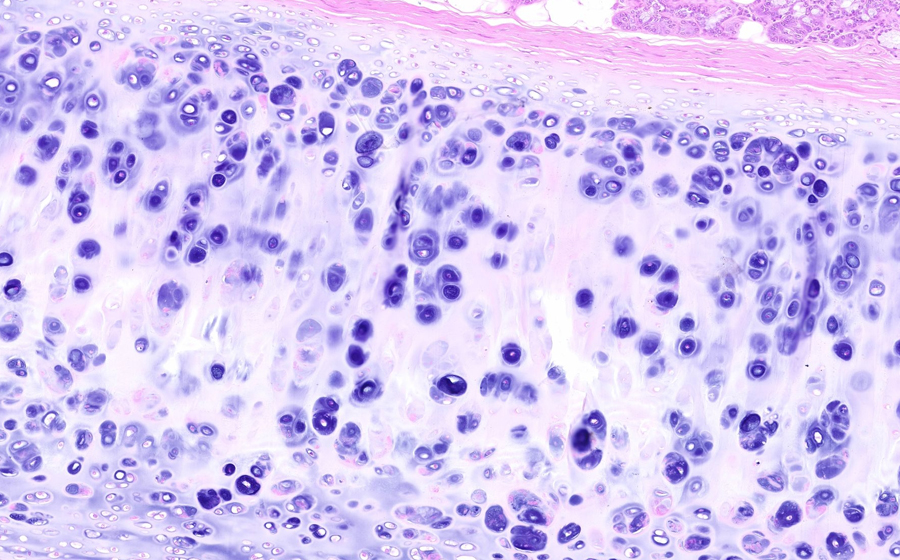
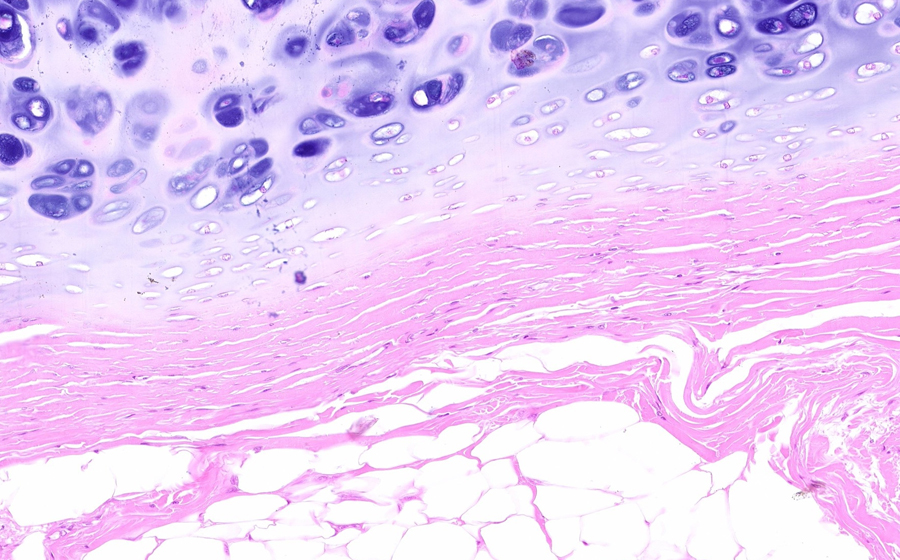
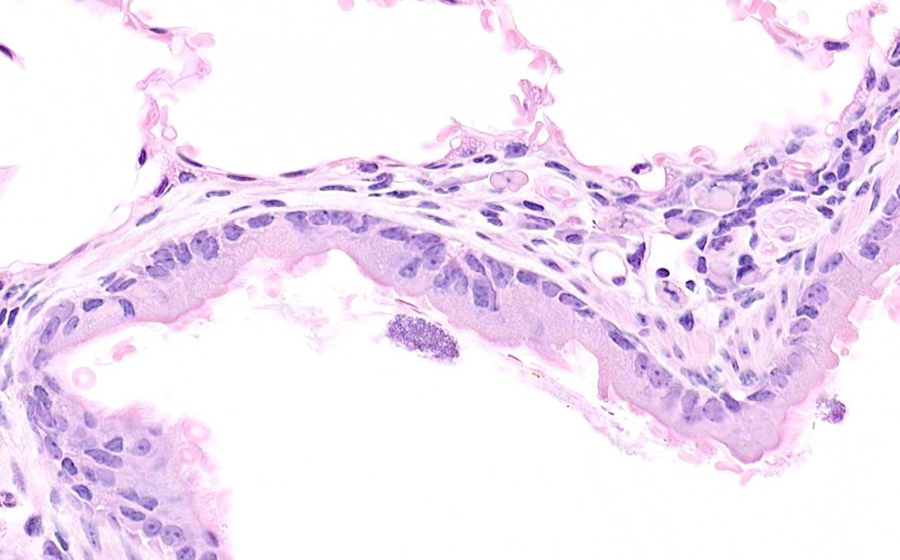
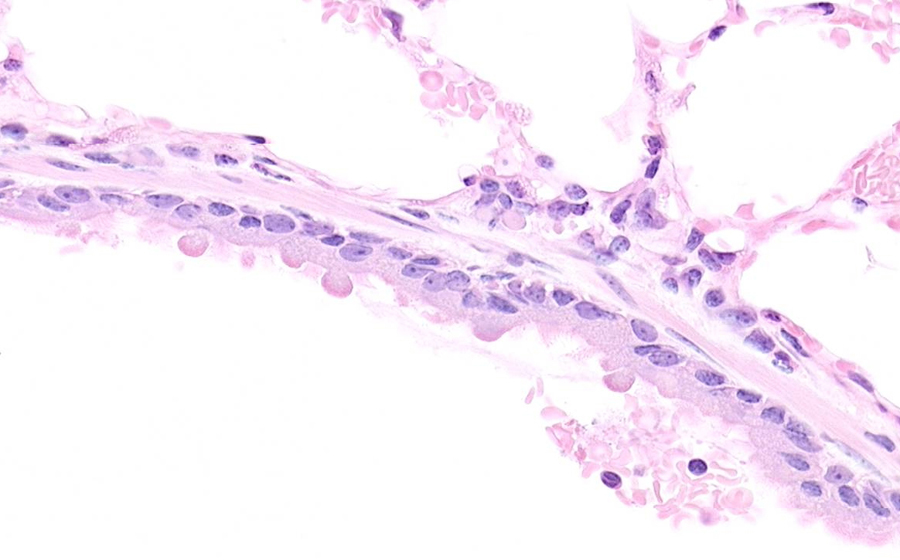
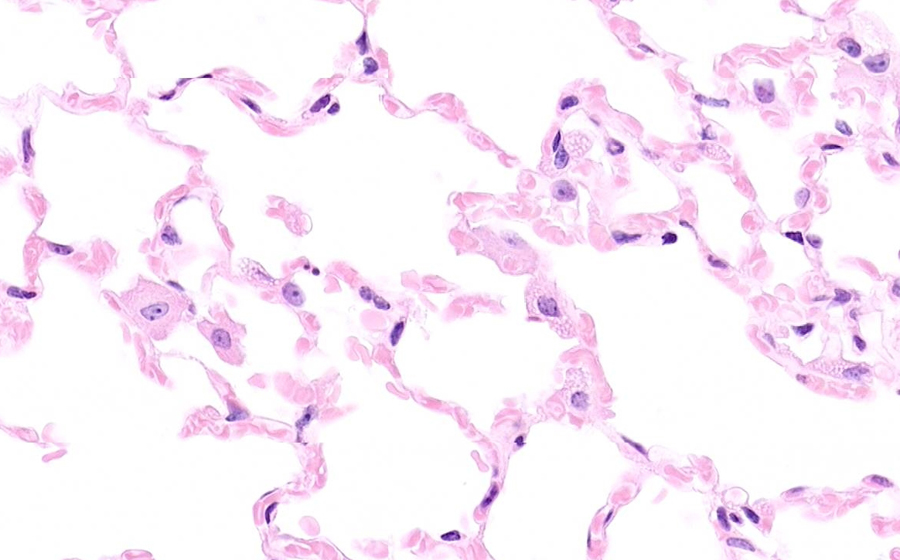
Image 2: One of the gross lung nodules is represented in this slide. From lower powers, the lung appears full and 'solid,' in that alveolar spaces aren't demonstrating the normal delicate quality imparted by open airspaces. Scattered subpleural emphysematous airspaces are seen, and subpleural anthracosis is also present. Both eosinophilic and basophilic areas can be discerned at low power.
Upon magnification, alveoli show a mixture of changes. Some alveoli are distended by purulent inflammation, and the many neutrophilic nuclei impart relative basophilia. Other alveolar spaces contain fibrin present as delicate and stringy material. Still others have abundant eosinophilic and homogenous material indicative of edema fluid. Capillaries of the alveolar septae are markedly congested, as are the scattered arterioles. All of these features typify an acute inflammatory process, and given the gross distribution, bronchopneumonia is an appropriate designation for this pulmonary process. Bronchial structures are not well identified in this autopsy slide, but are present as seemingly detached or free-floating strips of cuboidal-to-columnar epithelium, often present adjacent to intact vascular structures.
Question: Through what structure does bronchopneumonia spread within the lung?
Question: Through what histologic structure does lobar pneumonia spread within the lung?
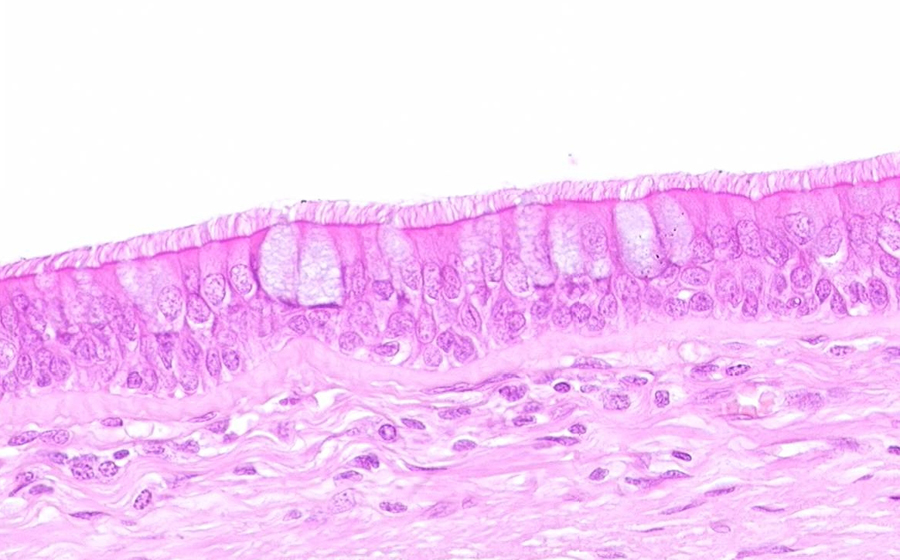
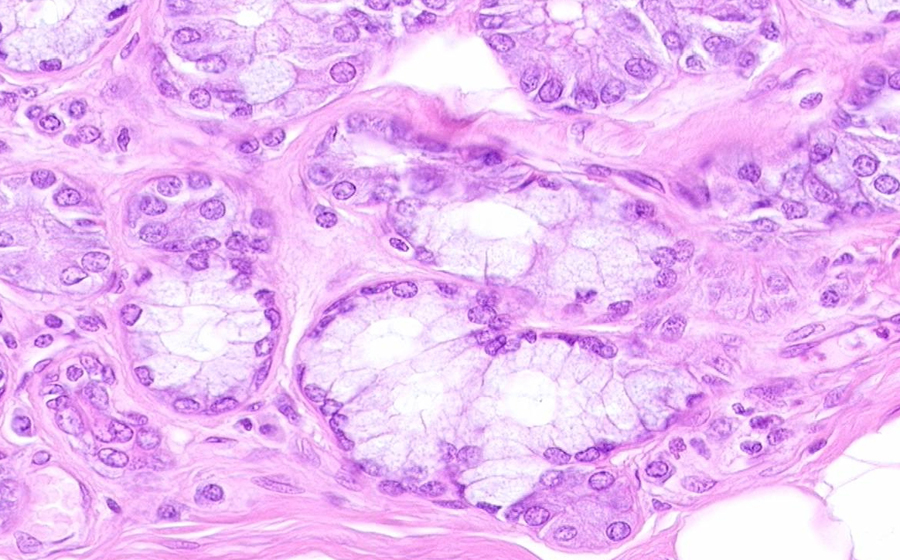
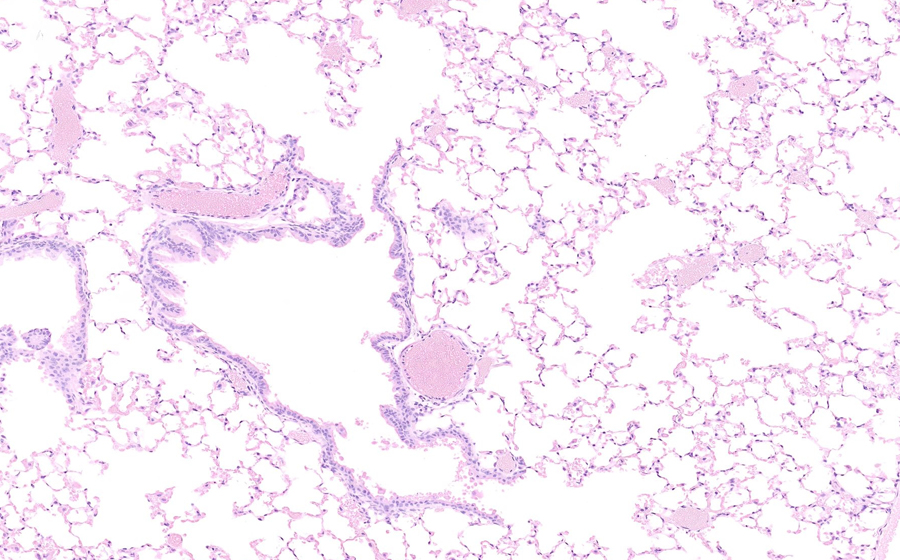
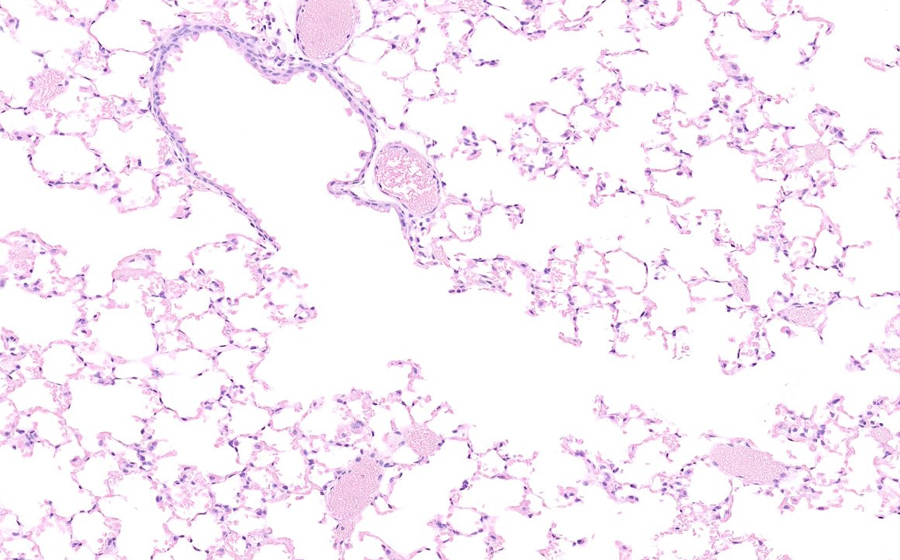
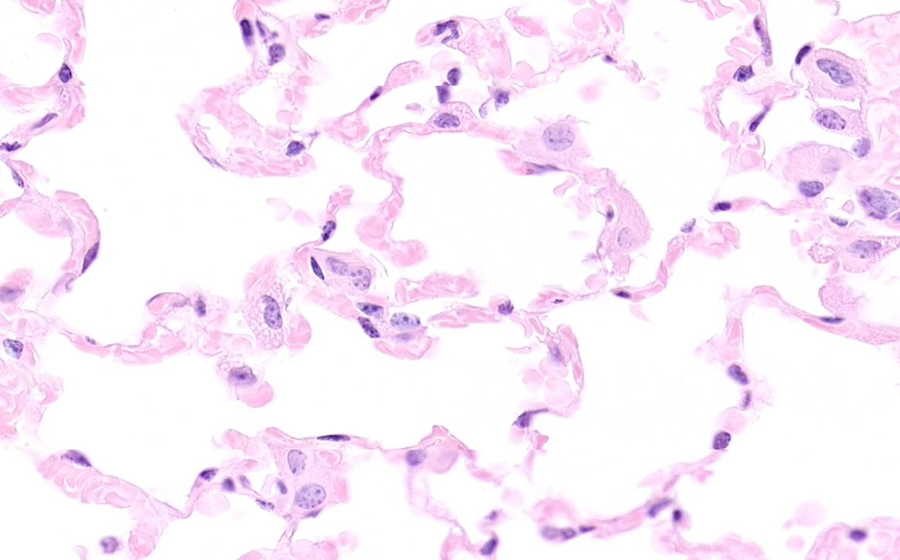
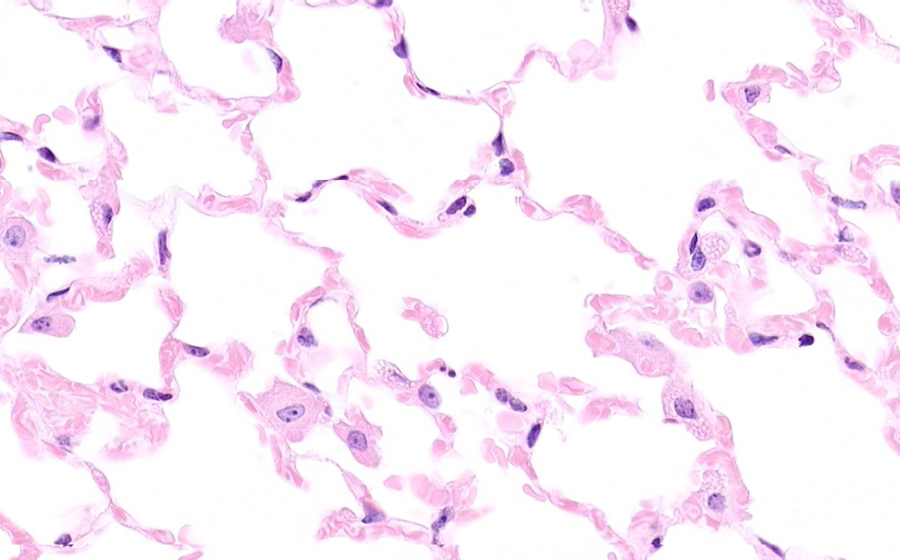
Image 3: In other areas of the lung away from the (consolidated) nodules, changes on this slide were apparent. Again from low power, the pulmonary parenchyma appears more solid than normal, although some open airspaces are evident.
The alveoli in this slide have a somewhat different quality than in the areas of bronchopneumonia. Neutrophils are scant, and the cellular infiltrate is composed of macrophages and pneumocytes, the latter of which are proliferating and 'active' appearing. Also prominent are characteristic hyaline membranes which can be seen in many alveoli as the hyaline-appearing, intensely eosinophilic material lining the alveolar space. Hyaline membranes consist of fibrin-rich edema fluid mixed with cytoplasmic and lipid components from epithelial cells and pneumocytes. Alveolar septae are also thickened, septal capillaries may show mild congestion, and an intraseptal lymphocytic infiltrate can be seen. These changes define the pathology of diffuse alveolar damage.
Question: Given the alveolar space changes and alveolar septal changes, what would be the expected impact on oxygen diffusion?